As Igor Rudan/Vecernji list writes on the 23rd of March, 2020, if we don’t go into quarantine, our healthcare professionals will not have to worry about a few dozen or several hundred people who are suffering from coronavirus more severely, which our system can handle, but several thousand of them, which it can’t. All of those differences are now our responsibility.
I have joined forces again with our renowned mathematician, Toni Milun, to explain through this text and the accompanying video why we now all have to stay in our homes for at least a month and strictly adhere to the quarantine guidelines.
Pandemics, like the world wars, are dynamic events with an uncertain outcome. In these times, things can quickly change from stage to stage. When encountering a new, unknown and invisible opponent such as this coronavirus, surprises are always possible. That’s why one should be careful, but one shouldn’t panic. Only those with ”cold” heads can make all of the important moves and respond to challenges at the right time, based on reliance on science and proven information.
On the one hand, the virus can always surprise us with its mutation. Random mutations of its genetic instructions can change the severity of the symptoms it will cause when causing an infection. They can also change the rate of its spread among the population. On the other hand, there are several lines of defense at our disposal that, depending on the behaviour of the virus, can be activated at the right time. Compared to the situation only three weeks ago, today, I have to make it clear that the epidemiology profession has significantly changed its perception of the danger of this new coronavirus.
By constantly collecting information from many countries, we now have a better understanding of the way it threatens us. I will try to explain here why the attitude of the profession has changed and why everyone now really MUST stay disciplined in their homes for at least a month.
I’ve written before that this is already the seventh coronavirus to try to adapt to the human species. The first four cause common colds and have been harmless to humans. The fifth, the SARS epidemic, however, was terribly dangerous. It killed as many as 10 percent of the people it infected. It expanded in 2002 from the Chinese province of Guangdong to more than 25 other countries, but was stopped everywhere on the front line(s) of defense.
The sixth one, the MERS epidemic, was even more dangerous. That killed as many as a third of those infected. It spread from Saudi Arabia to more than 25 other countries. But even then, it was stopped by the front lines of defense. These lines of defense include the isolation of patients and all of their contacts. When the epidemic of the seventh coronavirus, with COVID-19 as its causative agent, erupted in Wuhan in January 2020, it isn’t surprising that the epidemiologists’ interest was primarily focused on the death rate among those infected.
The reason is that previous death rates for SARS and MERS were so terribly high – 10 percent and 35 percent, respectively.
It was soon realised that the death rate among the most severe cases and hospital patients in Wuhan was about 5-10 percent when it came to this new coronavirus. However, it was only valid for the most severe cases that came to the hospital there, but not for anyone infected in the community. Infected doctors, like most patients in the population, had significantly milder issues. Therefore, it was necessary to determine as soon as possible the rate of death among those infected.
We got our first idea of the actual death rate of infected people when the work of Z. Wu and J.M. McGoogan was published in JAMA back at the end of February. It was based on a major report by the Chinese Centre for Disease Control, based on 44,672 COVID-19 positive patients in all Chinese provinces.
The authors showed that the death rate in the Hubei province was 2.9 percent, but they knew it was unrealistically high. This is because, at the earliest stage of the epidemic, the overwhelmingly severe cases that came to hospitals were tested, and there was no time at the height of the epidemic to test many in the community. A much more realistic estimate, therefore, was among those who tested positive outside the province of Hubei, on the front lines of defense of all other Chinese provinces. This death rate was 0.4 percent.
This means that for every 200 people with COVID-19, if given adequate medical care, only one person would die, or even less than that. Confirmation of that came from South Korea, where an unusual incident occurred. A community epidemic happened there, behind the front lines of defense. The authorities there went forward with en masse testing. Thus, the path of the virus among the population was constantly monitored and all the infected were isolated.
For such a very deep first line of defense, South Korea also had enough money, experience and all the other necessary facilities. 10,000 people were tested daily. Based on the first 140,000 tests, the rate of deaths in the community was estimated to be about 0.6 percent, again – one in two hundred, and quite similar to the estimate for all Chinese provinces outside of Hubei. These two figures are also very close to the estimate I made on March the 1st, that is, when spread among the community, COVID-19’s death rate should be between 0.5-1 percent.
In addition to the death rate among all those infected, it was also important for epidemiologists to know what the chances of a cure for all those who end up in hospitals are. It’s important to evaluate these prospects when the patients aren’t treated in the face of a booming epidemic and during an overload of local hospitals, and the situation in which entire medical teams are infected, but in conditions of being well prepared.
We learned these outcomes from the work of W. Guan et al., Published in the NEJM magazine. On February the 28th, they released a series of 1099 patients with laboratory confirmed COVID-19 infections from 552 hospitals in 30 provinces in China. This was a representative pattern of hospital treatment outcomes for China, in an environment where adequate care could be provided to all those infected. The estimated mortality rate of those with COVID-19 who end up in hospital was 1.4 percent, which was indeed much less than the first experiences in Wuhan.
Based on these two key pieces of information about COVID-19 – that is, in the community, it can lead to the death of only one in 200 infected people and that it kills one in 50 to 100 hospitalised people in hospitals – the epidemiology profession had its breath taken away. It no longer seemed to anyone that we were dealing with such a dangerous infection here. This is evidenced by the reactions of the world stock exchanges: Dow Jones was at 24,720 points on February the 28th, and jumped to 27,087 points by March the 3rd, meaning that it gained 10 percent on the total value in just five days after mortality rates became clearer.
The reason is that stock market investors have been in constant contact with leading epidemiologists over recent days. They were interested in how the situation was developing hour by hour. The view of the epidemiology profession during those five days was that we were likely to suppress the COVID-19 pandemic soon. These were exactly the days when I found myself in Zagreb and gave my first estimates to the Croatian media, after the first COVID-19 patients were recorded here.
The epidemiological profession’s view at the time was that the primary epidemic, in the City of Wuhan and in the province of Hubei, had been in continuous decline from February the 8th until the end of February; that the first lines of defense were able to stop the virus in thirty Chinese provinces, each with tens of millions of inhabitants; then that the virus was successfully halted on the front lines of defense in Japan, Taiwan and Singapore, the countries that have the highest human traffic with China.
In addition, even in South Korea, where an unforeseen epidemic occurred in the community, it was managed by intensive testing, with as many as 10,000 tests carried out per day.
The developments were then completely similar to the scenario already seen with SARS and MERS. The same scenario was repeated during the transition from February to March and with the third coronavirus, caused by COVID-19. There was also a primary focal point in the City of Wuhan in the Hubei province. It was suppressed by a large and strict quarantine, as the ultimate line of defense. All secondary foci were controlled by primary lines of defense. None of the epidemiologists thought at the time that EU and US countries wouldn’t be able to stop it in the same way.
The epidemic then seemed practically to be extinguished, and even the World Health Organisation delayed declaring COVID-19 a pandemic at all. It did it only about ten days later, that is, on March the 11th, because things had changed to such a dramatic extent. What, then, changed so much between the period of February the 28th and March the 3rd, when the epidemic seemed practically overpowered, and March the 11th, when the World Health Organisation declared a pandemic and the need for the absolute highest degree of caution?
According to the current understanding of the situation that the epidemiology profession can offer, after celebrating the Chinese New Year on February the 12th, about a week later, a number of Chinese workers employed in their textile industry, in northern Italy, returned to Italy. They were tested and recorded at the Italian airports by “first line of defense” measures. However, this seemed to be heard among the Chinese, so many began avoiding direct flights from China to Italy, returning via other European airports that didn’t exercise such strict controls. The Italians, however, didn’t control flights from the EU. Because of this, an epidemic that no one knew about began to quietly spread in the smaller cities of Lombardy, where many Chinese workers live, and behind the Italian line of defense.
There are many people living in northern Italy who went skiing in late February and early March. Across European ski resorts, they spread the infection enormously to the Swiss, French, Austrians, Germans and Spaniards, as well as citizens of many other countries in northern and western Europe. This is probably also because the spread of coronaviruses is generally favoured by lower temperatures. The current picture of the spread of the epidemic and of the hardest hit countries is in line with these developments.
As I described above, from March the 3rd to the present in many EU countries, most notably in Italy, which was one week ahead of the others, the number of infected people started to increase at an incredible rate. If the virus breaks through the first line of defense, we know that its growth will be exponential, but the human brain can hardly understand what that really means. In linear growth, anything added in the fifth week of expansion will represent one fifth of all cases so far. In the tenth week, a tenth. We know that and it is logical.
But when it comes to exponential growth, everything added up in each coming week will account for the vast majority of all cases, and anything that has happened before will seem irrelevant compared to just one week previously. This is what Tony Milun explains in today’s video.
I wrote about the dangers of exponential growth and the need to introduce major quarantines in Europe on March the 8th, and offered the option of strict quarantine for Croatia on March the 12th. But I have the impression that even in mid-March, the leaders of some EU countries still didn’t understand what the real danger of COVID-19 was. Thus, this coronavirus doesn’t kill primarily because COVID-19 is medically particularly severe in most patients, but mostly because it spreads deliberately and rapidly among humans.
Because of this, this coronavirus is incredibly fast in generating a huge number of patients, about 5 percent of which end up in an extremely serious condition. If we were able to provide each of them with optimal care in a timely manner, almost all the seriously ill would be saved. But if everyone gets sick at the same time, we can’t give them all intensive care. That is why almost all of the severe coronavirus cases will die. This is the way this virus has been killing so many people in Italy. They could have tens of thousands of patients suffering severely who will not be able to have access to intensive care and respirators.
The reason for the deaths in Italy was not, therefore, the severity of coronavirus per se, but rather that no one had taken the danger of an exponential spread seriously, meaning that quarantine was declared too late and then people just failed to respect it.
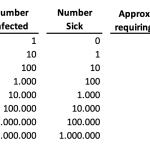
The incredible spread rate of this coronavirus is shown in the example in this table (below). The table shows what is happening to the population when the number of new cases is increasing by about 26 percent day by day compared to the previous day. This is quite a realistic scenario for many European countries these days.
The table first shows the days since the epidemic began. In the second column, the number of those infected with the virus is shown. It’s important to understand that those infected with the virus have not yet been discovered because they do not yet show any symptoms. Nonetheless, they can spread the infection over the next week while looking quite healthy. Only when they show symptoms of the virus a week later will they find themselves in the third column, as those who are “sick.” This means that when testing the number of patients on any given day, that we should expect that the actual number of infected people in the population is already ten times higher.
DAY 0 = 1 INFECTED = 0 SICK
DAY 7 = 10 INFECTED = 1 SICK
DAY 14 = 100 INFECTED = 10 SICK
DAY 21 = 1,000 INFECTED = 100 SICK
DAY 28 =. 10,000 INFECTED = 1,000 SICK
DAY 35 = 100,000 INFECTED = 10,000 SICK
DAY 42 = 1,000,000 INFECTED = 100,000 SICK
DAY 49 = 10,000,000 INFECTED = 1,000,000 SICK
Croatia has now passed day 21 and is moving towards day 28, but has declared a quarantine on time. Most EU countries have passed the 35th day and only then did they declare quarantine, so they can expect as many as 10 to 100 times more infected people than Croatia can. Italy declared quarantine when it was nearing its 42nd day and probably already had hundreds of thousands of people infected.
There are several other interesting things about this exponential spread of this infection. Namely, small countries are still in more danger than big ones are. The virus will spread exponentially among people using their mutual contacts, at the speed shown in the table above. It doesn’t matter how many inhabitants there are in the country in which it is expanding.
This is why smaller countries will be relatively more severely affected than large ones. For example, Italy, with its 60 million inhabitants, can spread the virus for 42 days, causing as many as 1 million people to become infected. Of these, about 5 percent, ie 50,000 of them, will become seriously ill. This is too large of a figure for their few thousand intensive care beds, and many cannot be provided with the assistance they need. Therefore, the Italian death toll from COVID-19 could be in the tens of thousands. However, not all the severely ill will die, because many will only require oxygen for their treatment and will not need a respirator.
This means that in Italy, as many as one million infected people could seriously endanger some 25,000 people. At least a few thousand of them will be assisted by intensive care, so the death toll would then be around 20,000. Even in such a scenario, it should be understood that only 1.6 percent of all Italians would get infected with COVID-19 at all, because Italy is a pretty large country.
In addition, 99.97 percent of Italians will survive it, which is important to understand for some future discussions on this topic. But, if COVID-19 had expanded exponentially in a much smaller country, it could have done significantly more damage there relative to the entire population, in relative terms. Things that happened in Italy should be put in an additional perspective. The scientific paper by A. and G. Remuzzi published in the March 2020 issue of Lancet showed that the average age of the first 827 deaths in Italy was 81 years and that more than two-thirds had diabetes, cardiovascular disease, cancer or were ex-smokers.
So these were the same people who probably would’ve died of the flu if they had not been vaccinated against it. Furthermore, in the scientific work of Rosan et al. Published in the 2019 International Journal of Infectious Diseases, influenza in Italy was attributable to 20,259 deaths in the 2014-15 season, and a total of 24,981 deaths in the 2016-17 season, even with vaccination. This means that the total number of deaths in Italy from COVID-19 could eventually be at least roughly comparable to those figures if the number of infected and dead continue to decline in the next few days.
However, taught by the experiences from back at the beginning of March, I’d also like to add that this is the view of the epidemiological profession on the state of affairs at the moment, to this day. Any new contingency – such as the realisation that the virus has indeed mutated and become more dangerous for younger people, or a repeated escape of the virus into an exponential spread, could change that view once again. Epidemics are dynamic and unpredictable events.
What we need to know now is that in the period from the 3rd to the 17th of March 2020, Croatia was still managing to maintain its first line of defense to a significant extent. It was at a time when the largest number of European countries already had exponential growth and uncontrolled spread in the community and reached a very large number of people with serious clinical issues that they would no longer be able to help. As you will see from the video by Toni Milun, in those fourteen days, Croatia had a 15-16 percent daily increase in the total number of infected people, while among the thirty other countries in Europe, Denmark was the worst with a 44-52 percent daily increase.
Then, after March the 17th, we introduced quarantine measures. If we’re to believe the numbers, because of all that has been done, we’d have to deal with at least 10 times less severely ill people than other Europeans, and as many as 100 times less than the Italians. But that will only be valid IF you’re all staying in your homes now and not leaving them for a month. If you ruin all the good that Croatian experts have done so far, which means with careless exposure and socialising in this situation, the virus will continue to spread rapidly among us.
Then, our health care professionals won’t just need to worry about a few dozen or several hundred people with a severe clinical picture, which, yes, our system can handle, but a few thousand of them instead, which it just can’t cope with. That difference depends entirely on us now. We need to remain patient in our homes for a month.
But then, just when everything was being done the right way, we were hit by this earthquake. I watched people go out into the streets after the earthquake struck, talking to each other in shock. Then, many people from Zagreb took the virus down to the south of the country with them, where we have significantly less capacity for intensive care. So, it was an incredible, totally incredible turn of events. Because of this, we can no longer predict the numbers. The number of infected people could be much higher than planned for by Croatian epidemiologists.
Instead of about 3000, it could now grow to a much larger number. All this is beginning to remind me of the finals of the World Cup two years ago. First, we played that game better than anyone could have hoped we would – that part would fit this period of “first line of defense.”
We had the lowest percentage increase in the number of cases in 30 countries across Europe. Then, an unfortunate own goal happened – because, from various European ski resorts, but also through the emergency services, the virus still found its way into Zagreb’s hospitals, exactly where we didn’t want it.
But then the equalisation came – we “locked” the country down and declared quarantine at the right time, thus preventing a large number of infections. But then came the earthquake in Zagreb, people went out onto the streets, the virus spread through conversation with one another, and then people carried it south, where we don’t have so much of a capacity for intensive care.
That’s why we all need to be Subasic now, but this time we simply have to defend the penalty. And all you have to do is stay home for a month.
This text was written by Igor Rudan and translated by Lauren Simmonds
Make sure to stay up to date with our dedicated section for all you need to know about coronavirus in Croatia.